- 1 About Health Impact Assessment
- 1.1 What is health impact assessment (HIA)?
- 1.2 Where does HIA sit
- 1.2.1 How is HIA different from other kinds of impact assessment?
- 1.2.2 How is HIA different from monitoring?
- 1.2.3 How is HIA different from evaluation?
- 1.2.4 Where does HIA sit in the planning and policy development process?
- 1.2.5 HIA in the Planning Process: When do you do it?
- 1.2.6 Health Public Policy
- 1.2.7 Healthy Urban Development Checklist
- 1.3 Glossary of HIA terms
About Health Impact Assessment
WE ARE UPDATING THE LINKS ON THIS PAGE – PLEASE BE PATIENT
What is health impact assessment (HIA)?
There are many definitions of health impact assessment (HIA). The most widely accepted one is from the Gothenburg Consensus Paper:
A combination of procedures, methods and tools by which a policy, program or project may be assessed and judged for its potential effects on the health of the population and the distribution of these impacts within the population. (ECHP 1999)
Other definitions emphasise that HIA:
- Assesses plans, project, program or policies before they are implemented.
- Predicts the health impacts of these proposals,
including:- assessing the severity and likelihood of the identified
positive and negative impacts; - determining whether these are direct or
indirect impacts, and - assessing the distribution of impacts.
- assessing the severity and likelihood of the identified
- Recommends mitigation measures:
- to maximise positive health impacts and minimise
negative health impacts; and - engage decision makers so that they consider health
impacts and the determinants of health in their
deliberations. (Harris et al 2007)
- to maximise positive health impacts and minimise
HIA can be undertaken on policies, programs or projects. It can also be undertaken on plans or other detailed strategic proposals.
Quality HIAs:
- Add value to decision-making processes
- Are undertaken only when there is a commitment on the part of proponents to act on the HIA’s recommendations.
- Are undertaken prior to the implementation of the policy, program or project that is being assessed.
- Assess the potential positive and negative impacts on health, including any unintended or previously unidentified potential impacts. They should also assess the distribution of the potential impacts.
- Define health broadly to include assessments of health hazards and risks as well as ways in which health and wellbeing could be promoted and the social forces that impact negatively on health reduced.
- Predict the impacts on populations both directly and indirectly affected by the proposal.
- Include equity and the distribution of impacts as a central concern.
- Engage key stakeholders in the formulation of recommendations.
What are the steps in HIA?
The steps in undertaking a HIA are:
- screening
- scoping
- identification of potential health impacts
- assessment of the potential health impacts
- decision-making and recommendations
- evaluation and follow-up
These steps do not have to be undertaken in exactly the same way and different types of proposals will require different methods as part of each step. It is essential, however, that these five steps are understood as integral to any health impact assessment – they “define” HIA.
The Steps of HIA
Source: Health Impact Assessment: A practical guide
Typology of HIA
There are four separate types of HIA than can be observed.
Mandated HIAs
Mandated HIAs are undertaken to fulfil a statutory or regulatory requirement and tend to place more importance on following a tightly prescribed process, with considerable emphasis on the scientific nature of methods used to identify potential health impacts. They usually adhere to more traditional positivist scientific conceptualisations of what constitutes evidence. They may also notionally be subject to legal challenge, though the extent to which this has happened to date is unclear and will likely vary in future depending on the jurisdiction in which they are undertaken. This form of HIA is most often conducted on major project proposals under environmental protection legislative requirements or regulations, although increasingly there is also provision for its discretionary use under public health legislation through powers granted to public health agencies.
Decision Support HIAs
Decision-support HIAs are usually undertaken voluntarily by, or in partnership with, the organisation responsible for developing the policy, program or project that is being assessed. The process for undertaking decision-support HIAs is often less formalised than for mandated HIAs, with a degree of flexibility around the methods and what is regarded as acceptable evidence of impacts. Whilst this form of HIA is usually undertaken on policies, plans or programs, there are examples of decision-support HIAs being undertaken on project proposals as well.
Advocacy HIAs
As HIA has become more widely understood there is increased interest in the use of HIA as an advocacy tool. Advocacy HIAs are undertaken by organisations and groups who are neither proponents nor decision-makers with the goal of influencing decision-making and implementation. Advocacy HIAs seek to reframe or challenge decision-making by ensuring that under-recognised health concerns are addressed in the design, decision-making and implementation of the proposal, in particular where the views of those most likely to be directly impacted have been under-represented. These HIAs usually take a clear position on the role of values and the ways in which “evidence” will be valued.
Community-led HIAs
One of the emerging areas of practice internationally are those HIAs conducted by communities to help define or understand issues and contribute to decision-making that impacts directly on their health. The purpose of community-led HIAs is to ensure the community’s health-related concerns are recognised and addressed. It is seen as an evidence-informed and practical by way in which communities can contribute to decisions — moving beyond a simple reliance on consultation to seek community views.
Source: Harris-Roxas, B.F. and Harris, E. (2011) Differing forms, differing purposes: A typology of health impact assessment. Environmental Impact Assessment Review, 31(4):396-403.
http://www.sciencedirect.com/science/article/pii/S0195925510000545
What’s the rationale for undertaking an HIA?
There are broadly four reasons that are given for undertaking HIAs:
- To identify hazards to health from the proposed development;
- To reduce or eliminate potential risks to health arising from these hazards and/or undertake risk communication as part of this process;
- To identify, and where feasible strengthen, the ways in which the proposed development can promote health and reduce health inequities; and
- To identify and address underlying social, environmental and economic impacts of the development that will have both direct and indirect impacts on health.
HIA enables decision-makers to enhance the potentially positive aspects and/or ameliorate the potentially negative aspects of the proposed policy, program, plan or project prior to implementation.
When should I do an HIA?
Not everybody who is developing a policy/program/plan or project needs to do a HIA Although the decision to undertake an HIA should not be solely based on whether resources are available, this aspect does need to be taken into account. The decision to undertake an HIA or not and the level of HIA (rapid, intermediate or comprehensive) should be undertaken as part of the screening process – which is the first step in the HIA process and the process where projects, policies or programs are selected for HIA.
The following issues should inform whether or not an HIA is required:
- Is there a clear proposal to be assessed?
- An initial assessment of the health impacts
- Is it possible to influence decision-making?
- The timing of the proposal being assessed
- An initial assessment of the potential links between the proposal and health
- An initial equity assessment of the proposal
- Whether the nature of potential impacts is well documented
- Whether other assessment tools are more appropriate
- Availability of resources and capacity
More information on determining whether an HIA is required is available in HIA: A practical guide.
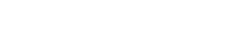
Conceptual Framework for Evaluating the Impact and Effectiveness of HIA
Ben Harris-Roxas
- Background
- About the Framework
- Conceptual Framework for the Impact and Effectiveness of HIA
- Considerations About the Framework
- So What?
- Further Information
- References
Background
Health impact assessment (HIA) is increasingly recognised internationally as a mechanism to ensure that the potential health benefits of policies, programs and projects are maximised and that potential negative health consequences and health risks are minimised (WHO 2008a, WHO 2008b, IFC 2006). HIA has also been on the public health agenda in Australia and New Zealand for more than 15 years, though its use has been limited. This is changing however, as indicated by activity by the Australian Commonwealth Government, the New Zealand Government, every Australian state to develop HIA (CHETRE 2008, Mahoney 2005). In New South Wales provisions for HIA’s use have been incorporated into a number of government strategies including the recent State Health Plan (NSW Health 2007b, NSW Health 2007a).
Despite HIA being cited as a mechanism to improve consideration of health and health inequities in planning and implementation (Acheson 1998, WHO 1997) reviews have found that there has been only limited evaluation of the impact of HIA on decision-making and implementation (Taylor & Quigley 2002, Harris-Roxas et al 2004). The considerable challenges in evaluating HIA have been acknowledged in the literature (Quigley & Taylor 2004, Cashmore et al. 2004). Decision-making processes, contexts and the policies that are subjected to HIAs vary markedly, making it difficult to develop a “one size fits all” approach to evaluation (Wismar 2004, Wismar 2007), and it seems likely that efforts to strictly codify HIA would actually impair its effectiveness and usefulness across a range of settings.
About the Framework
This conceptual framework for evaluating the impacts and effectiveness of HIA was developed following a systematic literature review and a review of severn completed HIAs, which included document analysis and 20 semi-structured interviews. It enables evaluators to conceptualise and represent the broad range of factors that influence the impact and effectiveness of HIAs. Publication of this study and the framework is pending.
Conceptual Framework for the Impact and Effectiveness of HIA
The framework has two major components – procedural elements and cross-cutting influences, with domains under each. These are outlined below.
Procedural Elements of the Framework
Parameters
These factors “set the scene” for the HIA. They may have been outside the process of the HIA itself but influenced the way the HIA was set up, the way the HIA’s recommendation were or were not be acted upon, and the reasons for the HIA to be conducted.
Decision-Making Processes
An evaluation should consider the structure and attributes of external decision-making processes, beyond the HIA itself, including the transparency and openness of these processes. How stable were these decision-making arrangements and how were they governed? What related political events occurred that influenced the HIA?
It is important to consider what timeframe was available to conduct the assessment, what deadlines were imposed, and why?
Decision-Makers
Who were the decision-makers responsible for acting on the HIA’s recommendations? (Note that these may be distinct from people responsible for making decisions within the HIA process itself) What role did they play in the commissioning and conducting the HIA? What were the personal characteristics of these decision-makers?
Additionally, what was the level of stakeholder and/or community interest in the proposal being assesses – support or opposition? To what extent were these “outsiders” involved in decision-making processes? For example did community representatives or stakeholders participate in planning or overseeing the development of the proposal being assessment
Type of HIA
An evaluation should detail the mandate or reason to undertake the HIA – was it mandated by law or regulations, was it being undertaken voluntarily for quality improvement, or was it being undertaken to advocate for changes to the proposal?
Was the HIA done as a stand-alone assessment or was it undertaken as a component of an integrated assessment or to contribute to other appraisal processes.
At what stage in the development of the proposal was the HIA undertaken? For example, was it undertaken while the proposal was at the conceptual stage or after a detailed proposal had been developed?
Inputs
These are the resources that were made available to conduct the HIA.
Proposal
What were the details of the proposal used to conduct the assessment? How much detail was included and how clear was it?
Capacity and Experience
How much experience and expertise did the assessors and steering group members have in conducting HIAs? What other skills and expertise were available? How much expertise and knowledge did the assessors and steering committee have in the proposal topic/area? Was there technical support available to undertake the HIA, including support for the HIA process or for specific data-gathering exercises?
Resources
What financial and human resources were made available to conduct the HIA, including voluntary and in-kind contributions.
Time
How much time was available to conduct the HIA?
Organisational Arrangements
Were there any existing partnerships or inter-organisational arrangements between stakeholder involved in the assessment? For example, was there a memorandum of understanding between the Ministry of Health and the agency developing the proposal?
Process
These are the factors relating to how the HAI was conducted.
Procedural Fidelity
Factors to be considered in evaluating an HIA include:
- Was a structured, stepwise impact assessment process followed? (see Health Impact Assessment: A Practical Guide for more information)
- Was the assessment conducted prospectively, i.e. before the proposal was implemented?
- Did the HIA include predictions about health impacts and identify the confidence limits on these predictions?
- Did the HIA examine differential impacts or health equity impacts? How?
- Were cumulative health impacts assessed? How?
- What guidance or best practice principles were followed?
- Was the precautionary principle referred to in the HIA – assessment or recommendations?
- Was the level of the HIA (desktop, rapid, intermediate, comprehensive – see FAQfor more information) appropriate for magnitude and significance of the impacts?
- Did the s cope of the HIA include pertinent environmental, social and economic determinants of health? How were these determined?
- Were potentially affected populations profiles in the assessment, including sub-populations and sub-groups?
- Was baseline information on relevant health indicators and relevant determinants of health reported?
- Were the impact identification methods rigorous and appropriate? Why/why not?
- What a assessment methods were used to assess the impacts identified? For example was a matrix used or some other method (see Health Impact Assessment: A Practical Guide)
- What were the nature and format of HIA recommendations, including recommendations for monitoring and management of health impacts? How were these developed?
Involvement of Decision-Makers and Stakeholders
What was the nature of involvement of decision-makers in HIA process and what was the level and nature of stakeholder involvement, including potentially affected communities.
Transparency
How was the process documented? Additionally how were decisions made during the HIA process and how was this documented, if at all.
Trade-Offs
Were areas of agreement and disagreement between sources of information/evidence identified? Were there areas of agreement and disagreement among the stakeholders involved in the HIA, including potentially affected communities, and how were these documented?
Review
Were stakeholder given the opportunity to review the draft HIA report before it was finalised? What changes were made because of this? was there any peer or independent review of the draft HIA report, and what changes were made in light of these?
Proximal Impacts
These are the things that changed most directly as a result of the HIA .
Informing decisions
Were potential health impacts considered by decision-makers?
Changing decisions and implementation
Observable changed including:
- Adoption of recommendations
- Implementation of recommendations
- Negative impact mitigation measures undertaken
- Positive impact enhancement measures undertaken
- Longer-term consistency of implementation and compliance with recommendations
- Management and follow-up of health impacts
Changes in Health
Were there observed changes in health indicators and determinants of health attributable to the proposal, incorporating monitoring activities? For example did community health outreach services associated with a major project improve the health of potentially affected communities? How?
Predictive Efficacy
Did health outcomes or changes in the determinants of health fall within predicted ranges? Note: This issue remains controversial, with some suggesting that the conditions for predictions or modeling will never match up with what ends up being implemented. Others suggest that predictive efficacy is not a meaningful criteria for evaluation – would a correct prediction imply the HIA was effective or successful? This is related to the perceived purpose of the HIA.
Achieving of Goals
Were the proposal’s goals achieved, even if the proposal was changed? For example, if the proposed dam was not built, was a way to generate the required energy found? The role of alternatives in the HIA, decision-making and implementation may play an important role in evaluating this factor.
In relation to the HIA, were it’s stated goals or objectives met? Were these explicit or implicit – see objectives.
Distal Impacts
These are more indirect changes to come about as a result of undertaking an HIA.
Understanding
A frequently cited benefit of undertaking HIAs are improvement in understandings – understandings of health and the determinants of health, health equity , the way other organisations work, the way decisions are made, the way other sectors use and value information, etc.
Participatory Learning
HIAs may lead to group learning – changes in understanding about health issues and the ways decisions are made, amongst a group of stakeholder or communities involved in the process. Did this occur? How? Why?
Influencing other activities
HIA is often described leading to other activities. Did the HIA lead to involvement in other planning activities and decision-making to include consideration of potential health impacts and the determinants of health? Did the HIA result in any ongoing within-organisation and between-organisation collaboration? Were there any related activities that “spun off”? Did the use of evidence to inform other decision-making processes change? For example, was evidence from the HIA used to inform other decisions and implementation?
Engagement
Did stakeholder engagement in this decision and decision-making processes change as a result of the HIA? Did stakeholder engagement in other planning activities or decision-making, change, including the involvement of potentially affected communities or groups? Did other relationships change as a result of the HIA?
Perception of HIA
Did the perception of the HIA’s usefulness by decision-makers and other stakeholders, including potentially affected communities, change? What was their perception of the HIA’s credibility? What determined this? How transparent sis they view the assessment and subsequent decision-making.
Cross-Cutting Influences in the Framework
Broader Context
HIAs are conducted in very different contexts across the globe. It is important that any evaluation of HA includes a description of the general governance, political and social context. Relevant recent and historical events should also be described and considered in the evaluation because these may play a significant role in determining whether an HIA is effective or not, independent of factors relating to how the HIA itself was conducted.
Presumptions about the nature of decision-making in general, beyond the HIA being evaluated, should also be considered. For example:
- What is the nature of policy development or planning processes in this context?
- What are the planning, information-gathering and consultation processes that usually inform decision-making in this context?
o Who are the stakeholders who generally influence decision-making in this context?
These considerations are particularly relevant in situations where HIAs are being conducted or evaluated by external consultants, who often start out with only a limited understanding of the context in which the HIA was conducted.
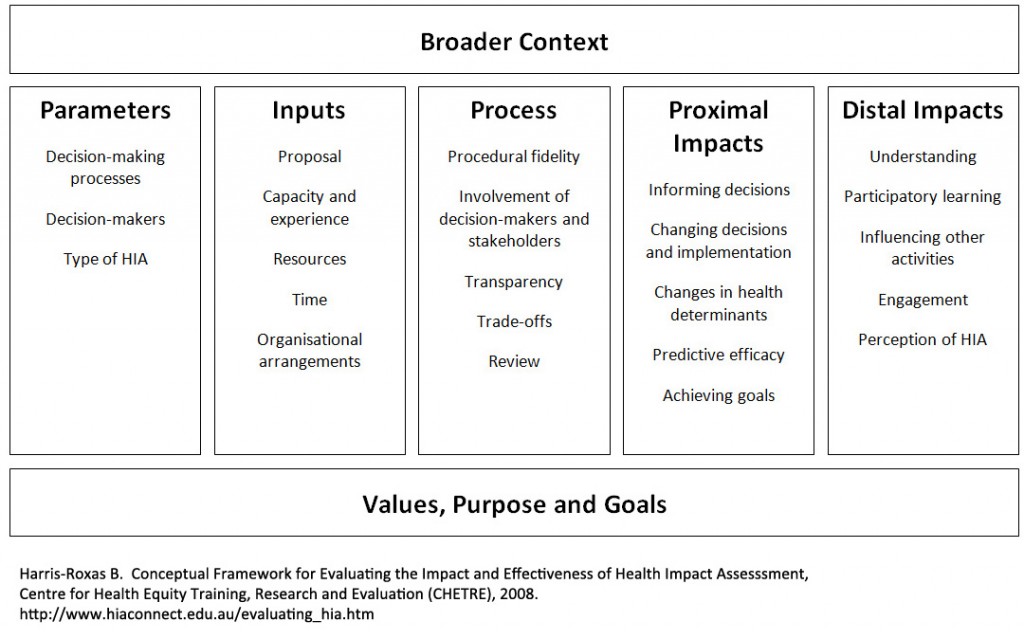
Values, Purpose and Goals
There is still considerable debate about the purpose of HIA, though as has been noted elsewhere this debate reflects the dynamic nature of the field of HIA rather than being a problem to overcome (Parry & Kemm 2004). The diagram below illustrates some of these varying perspectives:
Views on the Purpose of Health Impact Assessment
Click here for a full sized version of the image
Adapted from Cashmore M. The Role of Science in Environmental Impact Assessment: Process and procedure versus purpose in the development of theory, Environmental Impact Assessment Review, 24:403-426, 2004.
In light of these differences it is necessary to characterise the purpose of the HIA that is being evaluated.
An important criteria for evaluating any HIA is against its goals, stated or implicit. In order to do this it is necessary to what the HIA was trying to achieve in terms of:
- Decision-making:
- using information and evidence to inform decision-making;
- recommending enhancement and mitigation measures for decision-making;
- changing decisions and implementation;
- changing the extent and nature of public participation;
- generating debate; and
- Health:
- protecting health and minimising exposure to health risks;
- promoting health and enhancing health outcomes;
- promoting intersectoral action for health and healthy public policy;
- reducing health inequalities;
- changing understandings of health and determinants of health.
In addition to this it is necessary to describe the values and value-judgments underpinning the HIA, as this influences how an HIA is conducted. This includes:
- the personal values of those involved in the HIA and those responsible for acting on recommendations;
- the disciplinary values of those involved in the HIA and those responsible for acting on recommendations;
- the social and cultural values of those involved in the HIA and those responsible for acting on recommendations
- the role of evidence and what constituted evidence used in the HIA;
- the role of judgment and what constituted judgments in the HIA;
- how health was defined and what constituted a health impact and a determinants of health; and
- how equity and differential impacts are defined and what constituted a differential impact.
Considerations About the Framework
No HIA will address all elements of this framework, not should they. The framework provides an overview of the broad range of factors that can determine whether an HIA is successful or not – critical considerations in evaluating any HIA.
So What?
This framework provides:
- a conceptual basis for evaluating completed HIAs, moving beyond instrumental analysis of the direct effects of HIAs on decision-making and implementation to a more comprehensive understanding of the factors that enhance or reduce the effectiveness of an HIA;
- a basis for the development of future tools that may be used to plan future HIAs to enhance their impact and effectiveness; and
- an initial overview of which decision-making parameters, inputs and processes are linked with which proximal and distal impacts, which requires further investigation.
Further Information
For more information on evaluating HIA please look at the Evidence HIA Workspage.
For a full sized image of the framework click here.
For more information on the framework please contact Ben Harris-Roxas atb.harris-roxas@unsw.edu.au
References
Acheson D (1998) Independent Inquiry into Inequalities in Health, Stationery Office: London. Access Page
CHETRE (2008) HIA in Australia and New Zealand, Centre for Health Equity Training, Research and Evaluation (CHETRE): Sydney. Access Page
Harris-Roxas B, Simpson S, Harris E (2004) Equity Focused Health Impact Assessment: A literature review, CHETRE on behalf of the Australasian Collaboration for Health Equity Impact Assessment: Sydney. Access PDF
IFC (2006) Performance Standards on Social & Environmental Sustainability, International Finance Corporation, World Bank Group: Washington DC. Access PDF
Mahoney M (2005) Health Impact Assessment in Australia, NSW Public Health Bulletin, 16(7-8): 113-114. Access PDF
Parry J, Kemm J (2004) Future Directions for HIA in Health Impact Assessment(Eds Kemm J, Parry J, et al.), Oxford University Press: Oxford, 411-418. ISBN 0 1985 2629 6
Quigley R, Taylor L (2004) Evaluating Health Impact Assessment, Public Health, 118(8): 544-552 doi:10.1016/j.puhe.2003.10.012.
Taylor L, Quigley R (2002) Health Impact Assessment: A review of reviews, NHS Health Development Agency: London. Access Page
WHO (1997) The Jakarta Declaration on Leading Health Promotion into the 21st Century, World Health Organisation: Geneva, accessed 28 February.Access PDF
WHO (2008a) World Health Report 2008: Primary health care – Now more than ever, World Health Organization: Geneva. ISBN 9 7892 4156 3734. Access PDF
WHO (2008b) Closing the Gap in a Generation: Health equity through action on the social determinants of health, Commission on the Social Determinants of Health, World Health Organization: Geneva. ISBN 9 7892 4156 3703. Access PDF
Wismar M (2004) The Effectiveness of Health Impact Assessment, Eurohealth, 10(3-4): 41-43. Access PDF
Wismar M, Blau J, Ernst K, Figueras J (Eds.) (2007) The Effectiveness of Health Impact Assessment: Scope and limitations of supporting decision-making in Europe, European Observatory on Health Systems and Policies, World Health Organization: Copenhagen
Where does HIA sit
How is HIA different from other kinds of impact assessment?
Impact assessment:
is a process whereby predictions are made about the future consequences or impacts of changes being made or considered. The concept is general. Within a specific context, such as health effects, there may be a wide range of outcomes for which impacts could be assessed, such as death, GP visits, absence from work, etc. Different contexts may emphasise different outcome measures, but the constant theme is future prediction, and in particular prediction of differences in outcomes under different scenarios of change against the status quo. (Miller & Hurley 2003: 200)
Health impact assessment is only one type of impact assessment and the other kinds of impact assessment include:
- Environmental impact assessment
- Social impact assessment
- Mental Wellbeing Impact Assessment
- Integrated impact assessment
- Strategic environmental assessment
- Biodiversity impact assessment
Each form of impact assessment emphasises the specific contexts within which the impact assessment takes place. Social impact assessment prospectively assesses the potential social impacts of a proposal. For example in NSW social impact assessment are usually required for the introduction of a new gaming (alcohol & gambling) venues within an area.
The impacts addressed in an environmental impact assessment are wide ranging with “health effects” forming just one component. For example, an environmental impact assessment of a major project may look at the impacts on the broad socio-economic environment, including human health, archaeological and cultural significance of the site,, noise and vibration, air quality impacts, greenhouse gas emissions, transport impacts and even changes in amenity with the intent of assessing the overall impact of the project on the environment.
The origins of HIA lie partly in environmental impact assessment of major projects, along with a desire to address the social determinants of health and health inequities. The main differences between HIA as a standalone process (as opposed to how health has historically been considered in EIA) and other forms of impact assessment include:
- A different context – HIA (outside of EIA) specifically assesses the potential impacts on human health including impact of the social determinants of health on outcomes such as life expectancy, well-being, mental health and other morbidity measures. The impact of the physical environment on health will be addressed as part of this;
- Prospective impact assessment of proposed policies, plans, programs or projects – HIA is not limited to the potential impacts of a major development, such as the development of a new landfill site, but might assess the potential impacts of a proposed new taxation policy or a new chronic disease initiative on the health of a population. The importance of impact assessment of plans and policies has been recognised internationally through the rapid development of strategic environmental assessment.
- A core principle of HIA is equity – a HIA considers how potential health impacts are distributed in the population, differential health impacts and whether these impacts are potentially inequitable. (Harris-Roxas et al 2004)
How is HIA different from health needs assessment?
Health impact assessment (HIA) is different from health needs assessment in that it seeks to assess the potential health impacts of an actual proposal (policy, program, plan, or project) – there is something tangible to assess.
In contrast a health needs assessment is conducted to develop a comprehensive picture of health issues in a particular community, population group or geographic area. The findings of a needs assessment are usually used to inform the development and/or revision of a policy, program, project or plan, ie. to develop a proposal.
HIA might then be used to assess the potential health impacts of the proposal developed in response to the “needs” or issues identified through the needs assessment. In essence, health needs assessment is something to be done before an HIA.
How is HIA different from monitoring?
HIA is different from monitoring in that it seeks to assess (and predict) the potential health impacts of a proposal (policy, program, plan, or project) prior to implementation. In contrast monitoring is usually undertaken during and following implementation and the results of monitoring may be used to inform evaluation of an initiative.
An HIA’s recommendations might be used to inform the monitoring process, e.g. recommending the type of information and indicators that need to be collected to measure whether the potential health impacts eventuated. In terms of the planning or policy development cycle, monitoring is something that is done after HIA.
How is HIA different from evaluation?
HIA is undertaken prospectively – before the policy, program or project is implemented; unlike summative evaluation which is largely retrospective. HIA assists in the identification of negative and/or unintended consequences in advance of implementation. This provides an opportunity to ameliorate or amend the policy, program or project before implementation, saving not only resources but also maximizing the positive impacts from the proposed initiative.
Another key difference between HIA and evaluation is that it looks at the differential impact of the proposed policy, program or project (initiative) within the population. This includes (but is not limited to) looking at the distribution of impact in terms of:
- socioeconomic status,
- gender,
- age
- culture and ethnicity,
- location, including proximity and locational disadvantage (i.e. rurality, disadvantaged neighbourhoods, etc),
- existing levels of health and disability
(Harris et al 2007, Harris-Roxas et al 2004).
In contrast, the equity of impacts is not necessarily a principle that underpins evaluation.
While HIA and evaluation are different it is important to recognise they are also linked. Evaluations of existing policies, programs or projects can inform an HIA. An evaluation of an existing initiative might include scenarios that are used to predict what the consequences might be of amending or changing the initiative, enabling the use of an HIA approach. Also an HIA can provide information about the types of indicators that should be monitored during implementation and considered as part of the evaluation of an initiative.
- How is HIA different from Health in All Policies?
- How do the Healthy Environments Checklist and HIA ‘fit’ together?
For further information about other types of impact assessment see:
UPDATE REFS
HDA. Clarifying Health Impact Assessment, Integrated Impact Assessment and Health Needs Assessment, NHS Health Development Agency: London, 2004. Access PDF
Mindell J, Ison E, Joffe M. A Glossary for Health Impact Assessment. Journal of Epidemiology and Community Health, 57; 647-651, 2003.
Mindell J, Joffe M. Health Impact Assessment in Relation to Other Forms of Impact Assessment, Journal of Public Health Medicine, 25: 107-112, 2003.
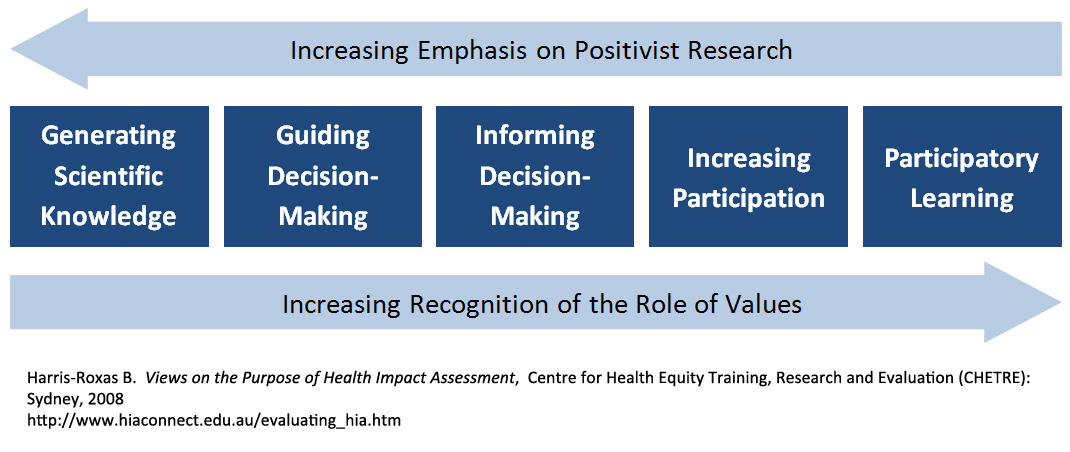
Where does HIA sit in the planning and policy development process?
There are many methods by which health impacts can be considered, including:
- Evaluation of health impacts and outcomes;
- Health needs assessment;
- Monitoring health indicators during implementation;
- Tools such as the Aboriginal health impact statement, equity lenses, health checklists; and
- HIA itself.
Knowing where HIA sits in relation to other methods for considering health impacts can assist in identifying when it is appropriate to use HIA. The following diagram outlines when an HIA should be undertaken in the planning or policy development process:
HIA in the Planning Process: When do you do it?
Source: Health Impact Assessment: A practical guide
HIA should not be used in place of sound needs assessment or planning but can be used to assess a draft policy/plan/program that has been developed as a result of needs assessment and planning. The HIA’s recommendations can then be used to strengthen the proposal as well as informing the development of indicators for monitoring, evaluation and follow-up.
Health Public Policy
Healthy Public Policy systematically and transparently incorporates concern for population health and well-being into the planning and implementation of policies, programs, projects and services by government, non-government and the private sectors by proposing actions to minimise health risk, promote health and reduce health inequity.
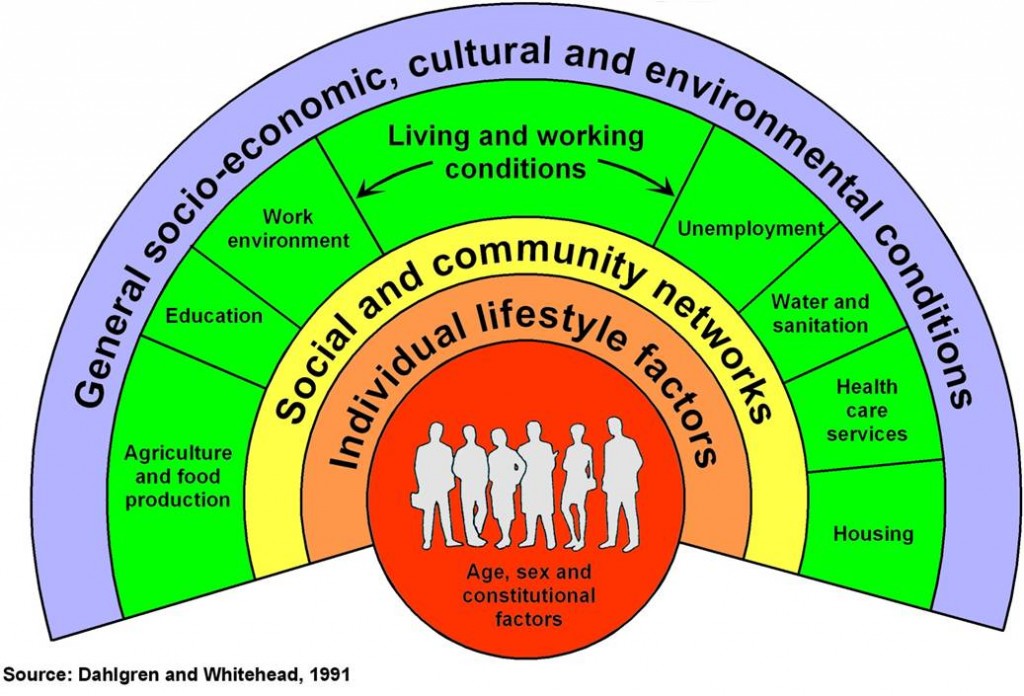
Determinants of Population Health and Wellbeing
Source: Dahlgren G, Whitehead M (1991) Policies and Strategies to Promote Social Equity in Health, Institute of Futures Studies: Stockholm
Healthy public policies improve the conditions under which people live, for exaxmple good housing, safe communities, access to adequate fresh water and nutrition, services, transport, education and employment. Health public policy aims to maximise the benefit of all policies on the health of populations.
This is important because many of the factors that affect health and wellbeing lay beyond the reach of health services and health policies.
Proportional Contribution to Premature Death
Source: Schroeder SA (2007) We Can Do Better: Improving the health of the American people, New England Journal of Medicine, 357(12): 1221-1228. doi:10.1056/NEJMsa073350
Health impact assessment (HIA) is a practical tool that can shift the rhetoric of healthy public policy into action. Instead of alluding to the interrelatedness of health and other sectors, HIA provides a transparent process for making these relationships clear.
Further Information
Reports
- Ståhl T, Wismar M, Ollila E, Lahtinen E, Leppo K (Eds.) (2006) Health in All Policies: Prospects and potentials, Ministry of Social Affairs and Health: Helsinki.Access PDF
- Blau J, Ernst K, Wismar M, Baro F, Gabrijelcic Blenkus M, von Bremen K, et al. (2006) The Use of Health Impact Assessment Across Europe in Health in All Policies: Prospects and potentials (Eds Ståhl T, Wismar M, et al.), Ministry of Social Affairs and Health: Helsinki, 209-230. Access PDF
- Wismar M, Blau J, Ernst K, Elliott E, Golby A, van Herten L, et al. (2006)
Implementing and Institutionalizing Health Impact Assessment in Europe inHealth in All Policies: Prospects and potentials (Eds Ståhl T, Wismar M, et al.), Ministry of Social Affairs and Health: Helsinki, 231-252. Access PDF - Kemm J (2006) Health Impact Assessment and Health in All Policies in Health in All Policies: Prospects and potentials (Eds Ståhl T, Wismar M, et al.), Ministry of Social Affairs and Health: Helsinki, 189-208. Access PDF
- Nilunger Mannheimer L, Lehto J, Östlin P (2007) Window of Opportunity for Intersectoral Health Policy in Sweden: Open, half-open or half-shut?, Health Promotion International, 22(4): 307-315. doi:10.1093/heapro/dam028
- Kemm J (2001) Health Impact Assessment: A tool for healthy public policy, Health Promotion International, 16(1): 79-85.
Articles
Healthy Urban Development Checklist
The purpose of the Checklist is to help build the capacity of NSW Health to provide valuable feedback to local councils, and other relevant organisations, on health issues in relation to urban development plans and proposals. It is intended that the use of the Guideline will facilitate strengthened partnerships and collaboration between NSW Health and urban planners and developers as part of NSW Health’s initiatives to promote healthy communities in NSW.
Healthy Urban Development Checklist
Glossary of HIA terms
Broader Model of Health
“Poor health cannot be explained simply by germs and genes. It is influenced by how we live and work and feel about our lives. Health, in its broadest sense, includes:
- Confidence and self esteem,
- A sense of belonging within a community, and
- Physical and emotional wellbeing.” (NPHS Wales 2003)
Comprehensive HIA
Comprehensive HIAs are intensive and often require additional data from diverse sources, including baseline assessment of health conditions. This level of assessment is rarely done in-house but usually by commissioning consultants.
Decision-Makers
The people who have control over the final content of the proposal and/or are responsible for its implementation, including the extent to which it is influenced by the HIA.
Determinants of Health
The range of personal, social, economic and environmental factors which determine the health status of individuals or populations.
Differential Impacts
Where impacts are distributed unequally across or within population groups.
Direct vs Indirect Impacts
Direct impacts affect the health of the population directly, for example exposure to pollutants (including noise) that a proposal may release in the air, water and soil. Indirect impacts affect the health of the population indirectly through the proposal’s influence on the determinants of the health, for example the effects a proposal might have on the local job market, access to local shops and amenities and the availability of public greenspace.
Enhancement Measures
Changes made to a proposal to increase the likelihood of positive impacts.
Environmental Impact Assessment
“A process of predicting… the effects of an action or series of actions on the environment, then using the conclusions as a tool in planning and decision-making.” (Prictard 1996)
Health
A state of complete physical, mental and social well-being and not merely the absence of disease or infirmity (WHO 1948).
Health Equity
Equity in health implies that ideally everyone should have a fair opportunity to attain their full potential and, more pragmatically, that no one should be disadvantaged from achieving this potential, if it can be avoided. (Whitehead 1990)
Health Hazard
An agent with a potential to create ill health (e.g., bacteria, toxins, chemicals).
Health Impacts
The effects, direct or indirect, of a policy, plan, program or project on the health of a population.
Health Inequality
Health inequality describes differences in health status usually between groups, such as the differences in health between older and younger people that occur due to natural factors. Unlike health inequity is is solely a statement of difference and does not involve a determination of whether that difference is unfair or unavoidable.
Health Inequity
Health inequity refers to differences in health status that are seen as potentially avoidable or unfair, as opposed to those that occur as part of normal life processes. (NSW Health 2004)
Health Outcome
A change in the health status of an individual, group or population which is attributable to a planned intervention or series of interventions, regardless of whether such an intervention was intended to change health status.
Health Promotion
Concerned with promoting health and wellbeing.
Health Protection
Concerned with protecting health from risks and hazards.
Health Risk
Indicates the extent to which the potential of a halth hazard may be realised.
Healthy Public Policy
“The main aim of health public policy is to create a supportive environment to enable people to lead healthy lives. Such a policy makes health choices possible or easier for citizens. It makes social and physical environments health-enhancing. In the pursuit of healthy public policy, government sectors concerned with agriculture, trade, education, industry, and communications need to take into account health as an essential factor when formulating policy. These sectors should be accountable for the health consequences of their policy decisions. They should pay as much attention to health as to economic considerations.” (WHO 1988)
Human Impact Assessment
Combined social and health impact assessments are sometimes called Human Impact Assessments (HuIA). This approach has been pioneered by STAKES in Finland.
Locational Disadvantage
Locations that are disadvantaged through lack of access to services and infrastructure or experience high levels of social disadvantage, such as rural and remote areas, outer metropolitan areas, and pockets of disadvantage within metropolitan areas.
Mitigation Measures
Measures to reduce the likelihood or severity of negative impacts.
Project Team
Those responsible for leading the work of the HIA, for report writing, and for framing the recommendations about modifications to the proposal.
Proponents
Those responsible for developing the proposal being assessed.
Social Impact Assessment
Social Impact Assessment (SIA) looks at the impacts of a certain decision on people, on the community or on society. These impacts are assessed in advance of implementation, to determine the changes the proposal will cause in people’s welfare or in the distribution of welfare.
Stakeholders
People involved in or affected by proposal development and implementation, drawn from public, private and voluntary sectors, and the communities or groups affected.
Steering Committee
Usually a Steering Committee is established between the screening and scoping steps to oversee the conduct and progress of the HIA. Establishing a steering committee is the core organising task of scoping.
Forming a steering committee involves balancing the need to make it small enough (a maximum of eight) to be manageable and making it large enough to include a
diverse range of perspectives and expertise. Useful areas of expertise for the committee are:
- the proposal topic,
- the potential population(s) affected,
- community involvement,
- public health expertose,
- negotiation skills,
- policy analysis,
- equity issues, and
- the social determinants of health.
“I’d recommend having representation on the committee from decision-makers and those who are in control of the proposal. The HIA we undertook was on a proposal being developed by the NSW Department of Planning. Having representatives from the Department on the committee allowed recommendations to be better tailored to the language and approach of the department.” (Harris et al 2007)
Unanticipated Impacts
Impacts that may not have been considered for various reasons, such as time, resources or professional orientation, during the development of a proposal.
Values
Establishing an HIA steering committee’s values and perspective on health early on in the proceedings of the steering committee helps to ensure that there is consensus on the scope of the impacts that will be assessed in the HIA. This involves answering questions such as:
- How will health be defined?
- How will health equity be defined?
- What specific groups, communities or populations will be considered in terms of differential impacts?
- How will evidence be valued and evaluated?
- How will competing or conflicting evidence be reconciled?
- How will recommendations be developed?
- What range of stakeholders will be consulted and how? (Harris et al 1997)
References
ECHP.Gothenberg Consensus Paper on Health Impact Assessment: Main concepts and suggested approach, European Centre for Health Policy, WHO Regional Office for Europe: Brussels ,1999. Access PDF
Federation of Swedish County Councils. Focusing on Health: How can the health impact of policy decisions be assessed? Landstrings Forbundet & Svenska Kommunforbundet: Stockholm, 1999. Access Guide
Harris P, Harris-Roxas B, Harris E, Kemp L. Health Impact Assessment: A practical guide, Centre for Health Equity Training, Research and Evaluation (CHETRE), University of New South Wales: Sydney, 2007. Access Guide
HDA. Clarifying Health Impact Assessment, Integrated Impact Assessment and Health Needs Assessment, NHS Health Development Agency: London, 2004. Access PDF
Miller B, Hurley J. Life Table Methods for Quantitative Impact Assessments in Chronic Mortality, Journal of Epidemiology and Community Health, 57, p 200-206, 2003.
Mindell J, Ison E, Joffe M. A Glossary for Health Impact Assessment. Journal of Epidemiology and Community Health, 57; 647-651, 2003.
Mindell J, Joffe M. Health Impact Assessment in Relation to Other Forms of Impact Assessment, Journal of Public Health Medicine, 25: 107-112, 2003.
Nilunger L, Schafer Elinder L, Pettersson B. Health Impact Assessment: Screening of Swedish governmental inquiries. Health Policy, 8(5): 30-32, 2002.
Scott-Samuel A, Birley M, Arden K. The Merseyside Guidelines for Health Impact Assessment. International Health Impact Assessment Consortium: Liverpool, 1998. Access Guide
References
Harris P, Harris-Roxas B, Harris E, Kemp L. Health Impact Assessment: A practical guide, Centre for Health Equity Training, Research and Evaluation (CHETRE), University of New South Wales: Sydney, 2007. Access Guide
NPHS Wales. Health Inequalities Impact Assessment Checklist: Guidance notes, National Public Health Service for Wales: Cardiff, 2003. Access Review
NSW Health. In All Fairness: The New South Wales Health and Equity Statement, NSW Health: Sydney, 2004. Access PDF
Pritchard D. Environmental Impact Assessment: Towards Guidelines for Adoption under the Ramsar Convention, 6th Meeting of the RAMSAR Contracting Parties: Brisbane, 1996. External Link
Quigley R, den Broeder L, Furu P, Bond A, Cave B, Bos R. Health Impact Assessment International Best Practice Principles. Special Publication Series No. 5, International Association for Impact Assessment: Fargo. Access PDF
Whitehead M. The Concepts and Principles of Equity and Health, World Health Organisation: Copenhagen, 1990. Access PDF
WHO. Adelaide Recommendations on Healthy Public Policy, World Health Organization: Geneva, 1988. Access PDF
WHO. Constitution of the World Health Organization, World Health Organization: Geneva, 1948. Access PDF